
Seeing Is Believing: The Benefits of Ultrasound for Patients and Providers
Blocked Fallopian Tubes? How Ultrasound Can Help Detect It
Blocked Fallopian Tubes? How Ultrasound Can Help Detect It
Most people trying to conceive assume their body “just works” — egg meets sperm, pregnancy happens. But one major hidden obstacle is the state of the tubes that connect the ovary to the uterus: the Fallopian tubes. When one or both are blocked, fertilisation is often frustrated before it really begins. The tricky part: blocked tubes often have no obvious symptoms.
In this article we’ll explore what blocking means, what causes it, and importantly how ultrasound (and related imaging) can help detect the problem so you can move toward a solution.
What Are Fallopian Tubes & Why Do They Matter?
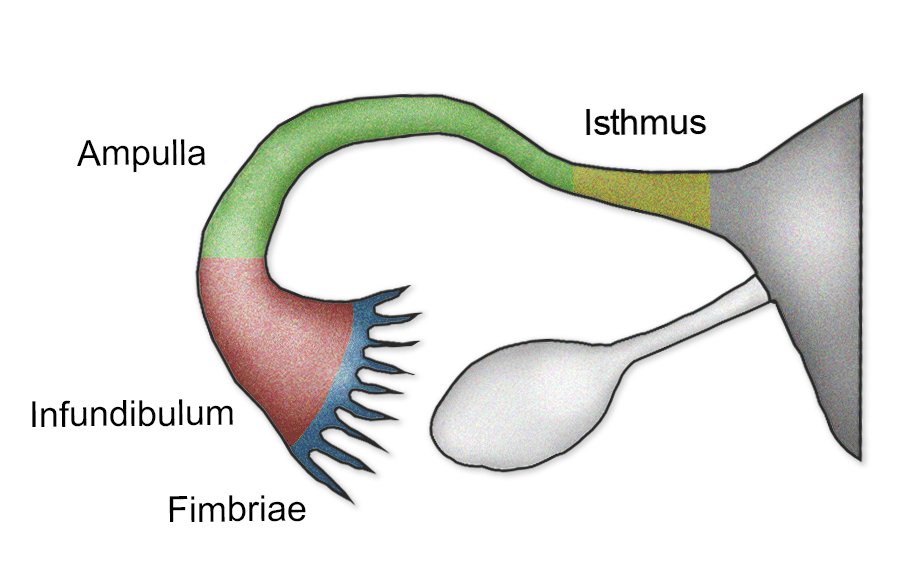
The fallopian tubes are slender ducts that carry the egg from the ovary toward the uterus and provide the space where sperm and egg meet. If they’re blocked, that journey gets halted — egg or sperm can’t make it, or the resulting embryo can’t make its way to the uterus for implantation.
According to fertility specialists, tubal problems are a significant cause of female infertility.
What Does “Blocked Fallopian Tube” Mean?
Partial or complete occlusion: A tube may be partially blocked (some flow possible) or completely blocked.
Hydrosalpinx: A specific form of blockage where fluid fills the tube, making it distended. This condition is visible on ultrasound in some cases.
Unilateral vs bilateral: One tube may be blocked (unilateral), or both (bilateral) — obviously bilateral matters more for fertility.
Why It’s Often “Silent”
Here’s the part you should emphasise for readers: many women don’t notice anything abnormal. No pain, no heavy bleeding, no classic “sign” of blockage. The first clue often comes when pregnancy isn’t happening.
So the absence of obvious symptoms doesn’t mean everything’s fine.
What Causes Tube Blockage?
Important for readership to understand they’re not necessarily “at fault”:
Past pelvic infections (especially Pelvic Inflammatory Disease / PID) or sexually transmitted infections.
Endometriosis (growth of uterine lining tissue outside the uterus) causing adhesions around the tube.
Previous pelvic or abdominal surgery causing scar tissue (adhesions) that interfere with tube opening or function.
Hydrosalpinx (fluid-filled tube) as noted above.
Rarely, congenital anomalies or tubal ligation (if applicable) may be a factor.
How Ultrasound Can Help — But With Caveats
Good news: Ultrasound (especially advanced techniques) can help detect tube problems.
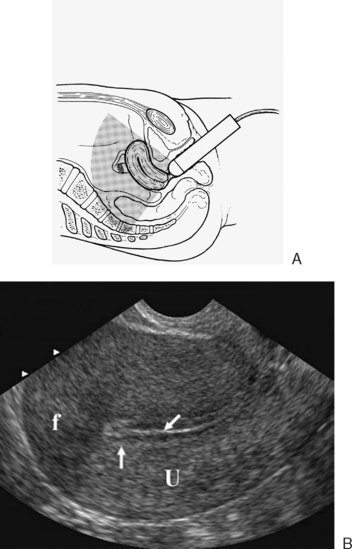
Caveat: Standard transvaginal ultrasound often can’t definitively diagnose tube blockade. Let’s unpack.
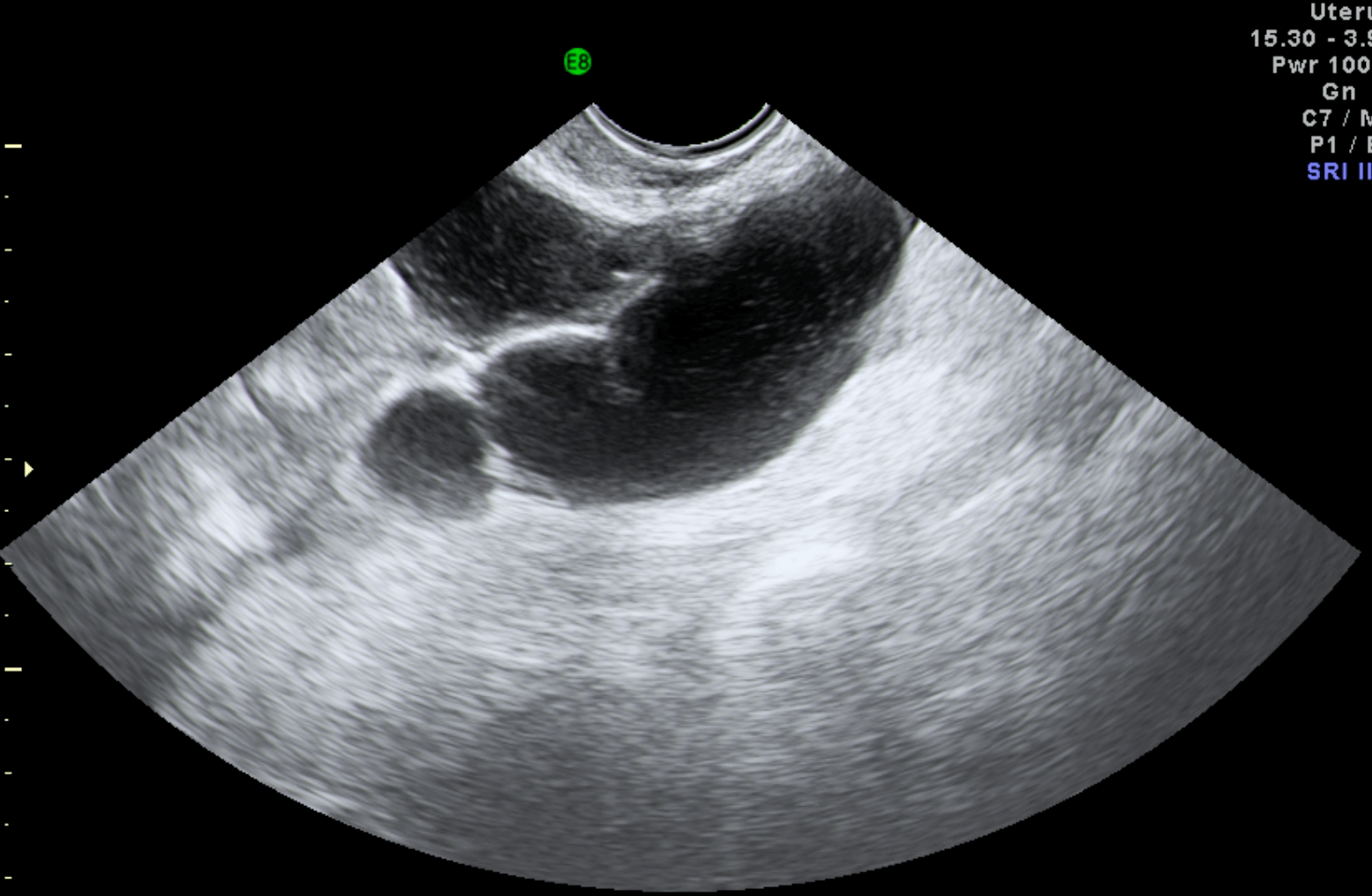
A transvaginal ultrasound might detect a hydrosalpinx — a fluid-filled, dilated tube. But if the tube is blocked yet not dilated, ultrasound may miss it.
There are specialised ultrasound procedures called Sonosalpingography or HSSG/HyCoSy (contrast fluid or foam introduced to assess flow) that help evaluate tubal patency without the radiation of a traditional X-ray.
Compare: the classical gold-standard for tube patency is Hysterosalpingography (HSG) — an X-ray with dye — because you can visualise the flow through the tubes.
So: if a patient’s just had a basic ultrasound, one cannot always conclude the tubes are clear. The imaging needs to be appropriate for tubal assessment.
When an Ultrasound Suggests a Problem — What to Look For
Here are findings on ultrasound that raise suspicion of tubal blockage:
A dilated tube filled with fluid (hydrosalpinx) appearing as a sausage-shaped or tubular anechoic structure.
Adnexal (near-ovary) fluid collections, or fluid build-up in the pelvis suggesting that flow might be impaired.
Absence of normal imaging flow or signs of contrast/foam not passing through on HyCoSy.
Thickened tube walls, or irregularities.
What This Means for Fertility and Next Steps
If one or both tubes are blocked, natural conception may be very difficult or impossible.
Some blockages may be amenable to surgical repair or laparoscopy; but in many modern fertility practices, especially when bilateral blockages exist, the recommendation may shift toward In Vitro Fertilization (IVF) because it bypasses the tubes altogether.
Even when tubes are open, their function matters (not just being open — but how well they carry eggs/fertilised embryos). Tubal damage can reduce success even if patency is demonstrated.
Emotional note: For many women this is a heavy moment. Diagnosis of tubal factor infertility triggers fears and questions. The blog should validate that feelings are real and professional support (medical & emotional) is essential.
Why Early Detection (Using Ultrasound/Advanced Imaging) Matters in 2025
With fertility trends shifting — later childbearing, more awareness of underlying reproductive-health issues — catching tubal problems earlier gives more options.
Advanced ultrasound techniques (HyCoSy, sonosalpingography) are less invasive and lower-cost than full surgical diagnostics.
Integrating fertility checks into health-care regimes is increasingly common; patients are more informed and expect clearer diagnostics.
For clinics like Atlanta Ultrasound, emphasising the availability of specialised ultrasound workflows (rather than just “general” ultrasound) is a competitive differentiator in 2025.
Tips for Readers Considering their Options
If you’ve been trying to conceive for 6–12 months (or 3–6 months if you’re older) without success — ask your doctor about tubal-patency testing.
Ask: “Can my tube function be assessed via ultrasound (sonosalpingography/HyCoSy) or will I need an HSG or other test?”
If ultrasound shows fluid-filled tubes (hydrosalpinx) or signs of dilatation, seek referral to a fertility specialist early.
Maintain good reproductive-health habits: Treat infections promptly, practise safe sex, discuss prior surgeries, and manage endometriosis or PID if present.
Connect with support — fertility journeys can be isolating; knowing you’re not alone helps.
Conclusion
Blocked fallopian tubes are a stealthy barrier to conception — often invisible until fertility becomes a challenge. Ultrasound alone isn’t always enough — but the right kind of ultrasound (and related advanced imaging) can be a powerful first step toward detection, diagnosis, and informed decision-making. For anyone on the fertility path in 2025, being proactive, asking the right questions, and choosing a clinic that understands tubal diagnostics is essential.
