
Seeing Is Believing: The Benefits of Ultrasound for Patients and Providers
Breast Skin Changes + Imaging: When Ultrasound Is Used in the Evaluation
Breast Skin Changes + Imaging: When Ultrasound Is Used in the Evaluation
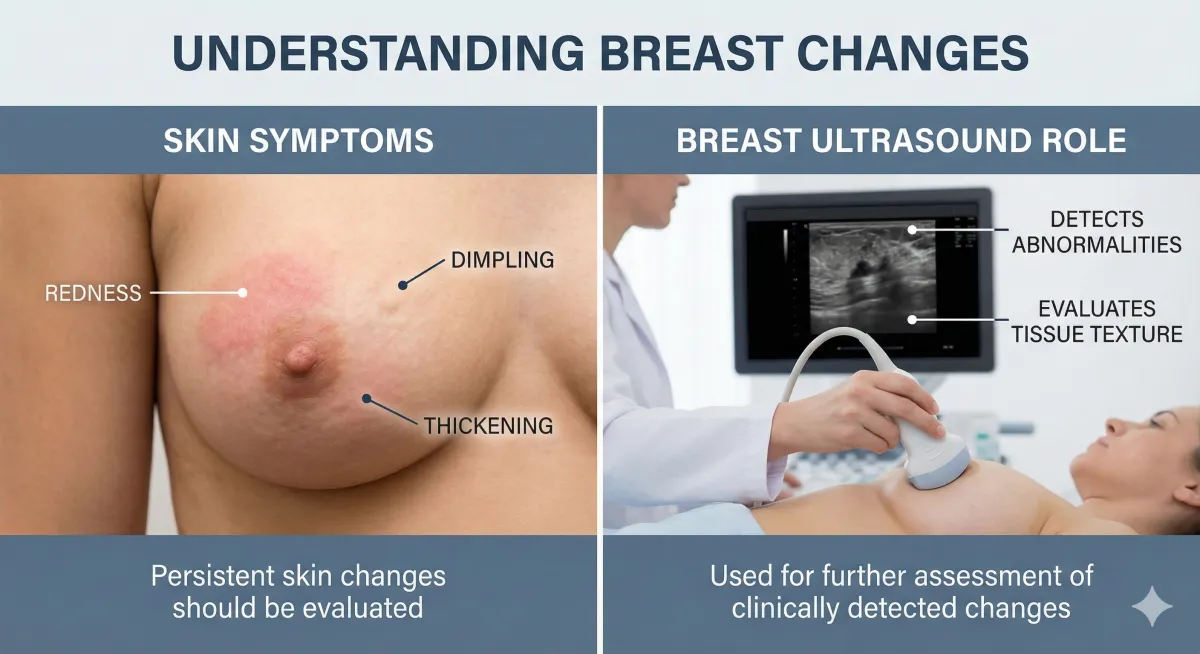
Breast skin changes can be caused by something minor (like irritation or an infection)… or something that needs urgent attention. The tricky part is that different conditions can look similar on the surface, so a proper evaluation matters.
Skin changes that commonly lead people to seek care include:
Redness or warmth
Swelling or “heaviness”
Thickening of the skin
Dimpling or “orange peel” texture (peau d’orange)
A persistent rash, scaling, or crusting (especially around the nipple/areola)
New nipple inversion or nipple changes

Don’t self-diagnose from Google Images
Here’s the blunt truth: you can’t reliably tell what’s going on just by looking at the skin. Some infections and some breast cancers can overlap in how they appear—so imaging is often used to help sort out what’s happening underneath.
When to get checked urgently
Contact a clinician promptly (same day or within 24–48 hours) if you have:
Rapidly spreading redness or swelling in one breast
Skin that looks pitted like an orange peel
Fever, chills, or severe tenderness (possible infection)
A new lump plus skin changes
A nipple/areola rash that doesn’t improve with basic treatment (like topical steroids)
Swollen lymph nodes in the armpit or near the collarbone
If symptoms persist after treatment for a presumed infection, clinicians typically escalate evaluation to rule out malignancy because the presentations can overlap.
The imaging “toolbox” for breast skin changes
Your provider may use one or more of these, depending on your age, symptoms, and exam:
Diagnostic mammogram (often a first step for many adults)
Targeted breast ultrasound (especially focused on the area of change)
Breast MRI (sometimes used when there’s high suspicion or to map extent of disease)
This article focuses on when ultrasound enters the picture.
So when is ultrasound used for breast skin changes?
1) When there’s skin thickening, swelling, or edema—and the goal is to look underneath
Ultrasound can evaluate skin thickness, subcutaneous (under-skin) edema, and the breast tissue below the skin. In conditions like inflammatory breast cancer, ultrasound commonly shows asymmetric skin thickening and subcutaneous edema, and may reveal masses that weren’t obvious otherwise.
Even when skin changes are thought to be inflammatory (like dermatitis or infection), imaging may be used because the role of imaging can be to evaluate for or exclude malignancy when symptoms don’t cleanly resolve.
Translation: ultrasound helps answer: Is there something deeper causing the skin to change?
2) When infection is suspected and we need to rule out an abscess
Breast infections (mastitis) can cause redness, pain, swelling, and warmth. Most cases are treated clinically. But if symptoms are severe, worsening, or not improving on antibiotics, ultrasound becomes especially useful.
Ultrasound can help differentiate:
Mastitis (more diffuse inflammatory changes) vs.
Breast abscess (a pocket of fluid/pus that may need drainage)
UCLA’s breast imaging teaching resource specifically notes ultrasound can help distinguish mastitis from abscess, especially with poor clinical response to antibiotics.
Why that matters: an abscess often needs a different plan than “just keep taking antibiotics.”
3) When there’s a lump (or a “thick area”) along with skin changes
If skin changes come with a palpable area, imaging is typically tailored to that abnormality.
Ultrasound is often central in lump evaluation, and what comes first can depend on age. ACR guidance for palpable breast masses notes:
Under 30: ultrasound is usually the initial imaging
30–39: ultrasound and diagnostic mammography/tomosynthesis are usually appropriate
40+: diagnostic mammography/tomosynthesis is usually initial, with ultrasound often added based on findings or recent imaging
Bottom line: if you feel something + see skin changes, ultrasound is commonly part of the workup.
4) When the nipple/areola has a persistent rash or eczema-like change
A scaly, red, painful, itchy rash on the nipple/areola that doesn’t resolve can sometimes be due to benign dermatitis—but it can also be seen with Paget’s disease of the breast, a rare breast cancer involving the nipple skin.
In Paget’s disease, ultrasound is often helpful when:
Mammography is negative, or
The patient reports a palpable lump
Ultrasound findings may include skin thickening at the nipple, areas of increased vascularity, discrete masses, or dilated ducts.
5) When inflammatory breast cancer is a concern
Inflammatory breast cancer (IBC) is rare but aggressive. It often causes rapid onset redness and swelling, sometimes without a distinct lump.
Ultrasound can show:
Asymmetric skin thickening and subcutaneous edema
Irregular hypoechoic masses (sometimes “hidden” on mammography)
Small anechoic spaces in the dermis reflecting lymphatic involvement
And the National Cancer Institute notes IBC symptoms can mimic infection, which is why evaluation matters and imaging may include ultrasound and MRI, plus biopsy when indicated.
6) When lymph nodes need a closer look (armpit/axilla)
Skin changes plus swelling or tenderness in the underarm can prompt an ultrasound of the axilla to evaluate lymph nodes—especially if there’s concern for infection spread or malignancy.
What to expect during a breast ultrasound
You’ll lie on an exam table; gel is applied to the skin
A transducer (probe) moves over the breast and sometimes the underarm
The exam is typically targeted to the area of symptoms
There’s no radiation (it uses sound waves)
Ultrasound is great at showing fluid collections, tissue architecture, and many solid massesbut it’s often used alongside other imaging depending on your situation.
What ultrasound can’t do (and why follow-up matters)
Ultrasound is powerful, but not magical. It may not detect certain findings as well as mammography, and results always need to be interpreted in context (your symptoms + exam + any other imaging).
The most important rule: If skin changes persist or worsen, don’t “wait it out.” Persistent symptoms after treatment should trigger further evaluation.
For those seeking expert ultrasound services, Atlanta Ultrasound offers quick, efficient, and comprehensive scans. Our team of skilled professionals is dedicated to providing you with the clarity and care you need.
Contact us today to schedule your ultrasound scan and take a decisive step towards understanding your health.
📍 Multiple locations in Metro Atlanta, GA
📞 Contact: 678-590-3300
🌐 Website:www.atlantaultrasound.com
Disclaimer: The content of this blog post, authored by a sonographer, is provided for educational and informational purposes only. It is not intended as medical advice, nor should it substitute for professional medical consultation, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition or health concerns.
